Hundreds more cases of potentially avoidable baby deaths, stillbirths and brain damage have emerged at an NHS trust, raising concerns about a possible cover-up of the true extent of one the biggest scandals in the health service’s history.
The additional 496 cases raise further serious concerns about maternity care at Shrewsbury and Telford hospital NHS trust since 2000.
The cases involving stillbirths, neonatal deaths or baby brain damage, as well as a small number of maternal deaths, have been passed to an independent maternity review, led by the midwifery expert Donna Ockenden. They bring the total number of cases being examined to 1,862.
They will also be passed to West Mercia police, which last month launched a criminal investigation into the trust’s maternity services. Detectives are trying to establish whether there is enough evidence to bring charges of corporate manslaughter against the trust or individual manslaughter charges against staff involved.
The extra 496 cases had not emerged until now because an “open book” initiative led by the NHS in 2018 asked only for digital records of cases identified as a cause for serious concerns. The vast majority of the 496 further cases were recorded only in paper documents.
The Ockenden review was ordered in 2017 by the then health secretary, Jeremy Hunt, after the families of two babies who died under the trust’s care raised concerns about their case and 21 others.
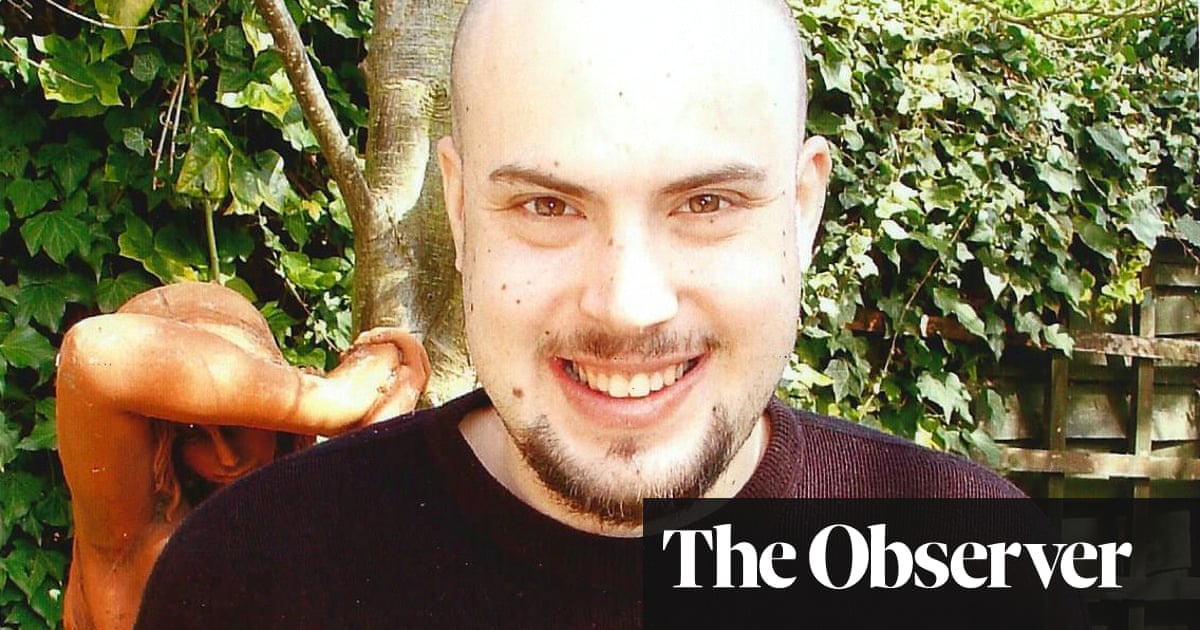
They include Rhiannon Davies, whose daughter Kate Stanton-Davies died in 2009 and who has been campaigning to force the NHS to reveal the true extent of the scandal.
Speaking to the Guardian, she said: “These extra cases definitely fuel my concern that someone involved in the open book review has not been entirely open.” Davies, who successfully campaigned against the NHS imposing an oversight committee on the Ockenden review, added: “We want no more adverse interference from any external bodies such as NHS England or the Department of Health on the Ockenden review team. They need to be left alone to get on with their work.”
The trust’s chief executive, Louise Barnett, issued an open apology to people in Shrewsbury and Telford. “Our standards have fallen short for many families and I apologise deeply for this,” she said. “We should have provided far better care for these families at what was one of the most important times in their lives and we have let them down.”
The extra cases mean the maternity failings in Shropshire could eclipse the Mid Staffordshire scandal, until now the worst in the history of the NHS. A review into that trust found that between 400 and 1,200 patients died as a result of poor care between January 2005 and March 2009.
A report by the Royal College of Obstetricians and Gynaecologists (RCOG) in 2018 into maternity care at the Shrewsbury and Telford trust said: “Neonatal and perinatal mortality rates will not improve until areas of poor/substandard care are addressed.”
A follow-up review published on Tuesday by NHS Improvement sharply criticised how the trust handled the RCOG’s criticism. It suggested it was more worried about public and media reaction to the RCOG report than patient safety.
It found the trust delayed publishing the critical report until it could provide assurances that improvements had been made. The follow-up review said: “It would have been more transparent to publish sooner.” It also found a “culture of defensiveness, denial and/or lack of openness that existed at the time in maternity services”.
The parents of Kate Stanton-Davies and Pippa Griffiths, another baby who died in the trust’s care in 2016, called for the current board to be replaced. In a letter to the chief inspector of hospitals, also released on Tuesday, they said: “We believe the board is complicit in the active prevention of change for the benefit of patient safety and therefore needs to be immediately sacked. How many times will it need to be told before it listens?”
Ben Reid, chair of the trust, said: “It is clear that internal scrutiny would have been improved if we had decided not to wait for the addendum to the report before placing it before the Board and the Quality and Safety Committee.
“Action plans were being produced within the trust but, without the oversight of the full governance process, that clearly wasn’t a robust enough response.
“We, as a trust, and I personally, have learnt a valuable lesson as to how we handle such reports in the future. I consider it my responsibility to take these lessons forward and ensure they are applied across the organisation.”
Ockenden hopes to publish interim findings later this year. She said: “The trust has worked closely with the review team throughout this process and have provided us with all requested information. By working together we have sadly identified a further 496 families as part of the review, who I am writing to this week.
“It’s now really important that we focus our efforts on getting all clinical reviews completed so that we can make meaningful recommendations to improve services and give families the answers they have asked for. We intend to have initial, emerging recommendations for maternity services published at the end of the year.
“In order to give ourselves the time to write the final report, any new cases that come to light from now on will need to go directly to the trust for them to consider, rather than them coming to the maternity review team.”
A spokeswoman for NHS Improvement, said: “NHS Improvement commissioned an ‘open book’ review specifically looking into the trust’s reporting of incidents and as more families came forward with concerns, the review’s terms were extended to encourage the trust to provide all relevant case notes and information.”