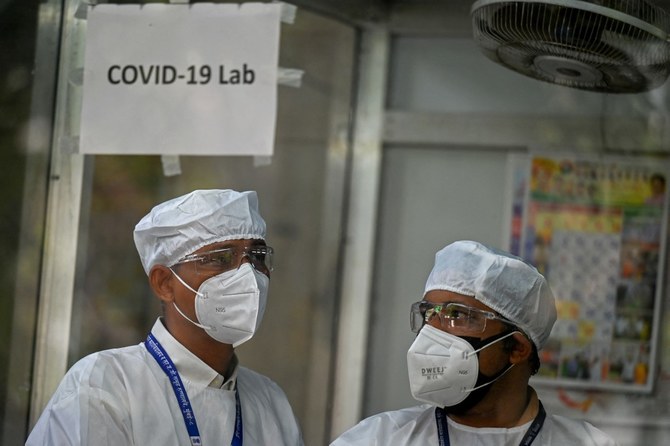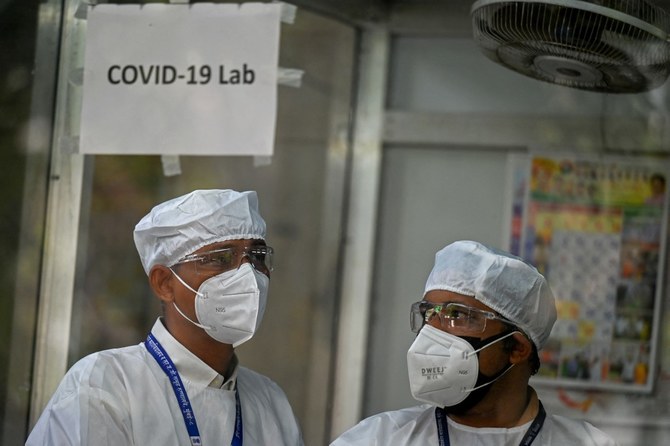
While COVID-19 restrictions are rapidly fading around the world, we are still reeling from the impact of the past three years. More than 6.8 million deaths from COVID-19 have been officially reported, but the true number may be closer to 15 million. There has been immense suffering and social and economic turmoil and the virus itself still poses a clear and present risk, with one in five Americans reporting ongoing “long COVID” symptoms.
Worse, COVID-19 is far from the last zoonotic disease with the potential to devastate the global population. Innumerable other viruses — many of which remain understudied — have been discovered in animals. Any of them could serve as a source of new human viruses, which often originate from repeat offender virus families such as coronaviruses, orthomyxoviruses and filoviruses. When viruses from these families show up in mammals or birds, there is always a risk that they could develop the potential to infect humans. And when that happens, globalization means that those viruses can spread faster than ever before.
A key challenge, then, is to discover and identify which viruses pose the greatest risks to humans. If we can detect a new human virus in the earliest days of a disease outbreak, we will have a much better chance of implementing the measures needed to prevent another global pandemic. To that end, a recent article in Science proposes setting up an experimental pipeline whereby researchers can test animal viruses for four crucial properties consistent with human infection.
By identifying the viruses that pose the highest risk for zoonosis (transmission across species), we can then rapidly roll out diagnostic panels to detect new human infections. Serology- and polymerase-chain-reaction-based diagnostics are currently the most practical solutions for healthcare settings around the world. But they are pathogen-specific, so they are effective only when clinicians and scientists know which pathogens they should be testing for.
An animal virus needs four essential biological properties in order to infect humans: it must use the human version of its cellular entry receptor to gain access to human cells; it must use human intracellular proteins to replicate and exit human cells; it must overcome humans’ innate immune responses; and it must evade existing human adaptive immunity functions such as antibodies and T cells.
COVID-19 is far from the last zoonotic disease with the potential to devastate the global population
William A. Haseltine
Animal viruses that have most of these properties — such as primate arteriviruses — obviously warrant targeting by new diagnostic tools. Such tests can be grouped into regional panels for use in diagnosing unusual or unattributable human illnesses, as well as to monitor healthy populations for virus surveillance purposes.
The first zoonotic property — an ability to enter human cells — is often the easiest to study because we can test the surface protein of an animal virus by engineering it onto a reporter virus (a reporter virus genome lacks genes essential for viral replication, making it safe for research and surveillance purposes). This method has been shown to demonstrate that some poorly studied tibroviruses from the Rhabdoviridae family can enter human cells, though their multiplication within human cells is uncertain.
The ability to multiply — the second biological property viruses need to infect humans — involves a complex process that requires interactions with several intracellular host proteins. Even a single incompatibility can prevent an animal virus from multiplying in human cells.
There is scarce research on the third property: how animal viruses interact with human-innate immunity beyond the interferon response. This is a first line of defense against virus infections. It functions by generating an intracellular environment that restricts virus replication and signals the presence of a viral pathogen to the adaptive arm of the immune response. Further study is needed to determine, for example, why some ebolaviruses can multiply in human cells, yet rarely infect humans in nature. In these cases, there seem to be powerful innate immune mechanisms protecting animals, including humans, from cross-species transmission.
The final property is an ability to overcome existing human adaptive immunity, such as neutralizing antibodies and cytotoxic T cells. While human responses raised against one virus can be tested for reactivity against a second virus, it is unknown how much cross-neutralization would be enough to protect humans from infection or severe disease if exposed to potentially zoonotic viruses.
To detect outbreaks at their onset, clinicians and scientists must be able to track animal viruses in human populations. Yet our healthcare systems currently struggle to provide testing even for well-understood viruses. We urgently need greater investments in universal and accessible healthcare, which would have the added benefit of enhancing our virus surveillance abilities.
But in addition to more comprehensive surveillance protocols and stronger health systems, we also need to address the underlying causes of zoonotic disease emergence, such as deforestation, the wildlife trade and climate change. While implementing a comprehensive pandemic prevention framework will require significant investment, the cost of inaction is sure to be far higher. Population growth, expanding urbanization and encroachments on nature, and the resumption of regular air travel mean that infectious disease outbreaks will continue to plague us.
They already are. New cases of highly pathogenic avian influenza across the US and in other parts of the world are a wake-up call. We should always assume that the next pandemic is closer than most people think.
William A. Haseltine, a scientist, biotech entrepreneur and infectious disease expert, is chair and president of the global health think tank ACCESS Health International. Copyright: Project Syndicate, 2023.