The South African health department says the reduced cost of a new anti-HIV injection is still three times more than it can afford to pay.
The UK-based drug company ViiV Healthcare has lowered the price from 729 rand per shot (£32) to between 540 and 570 rand (£23.66-£24.97).
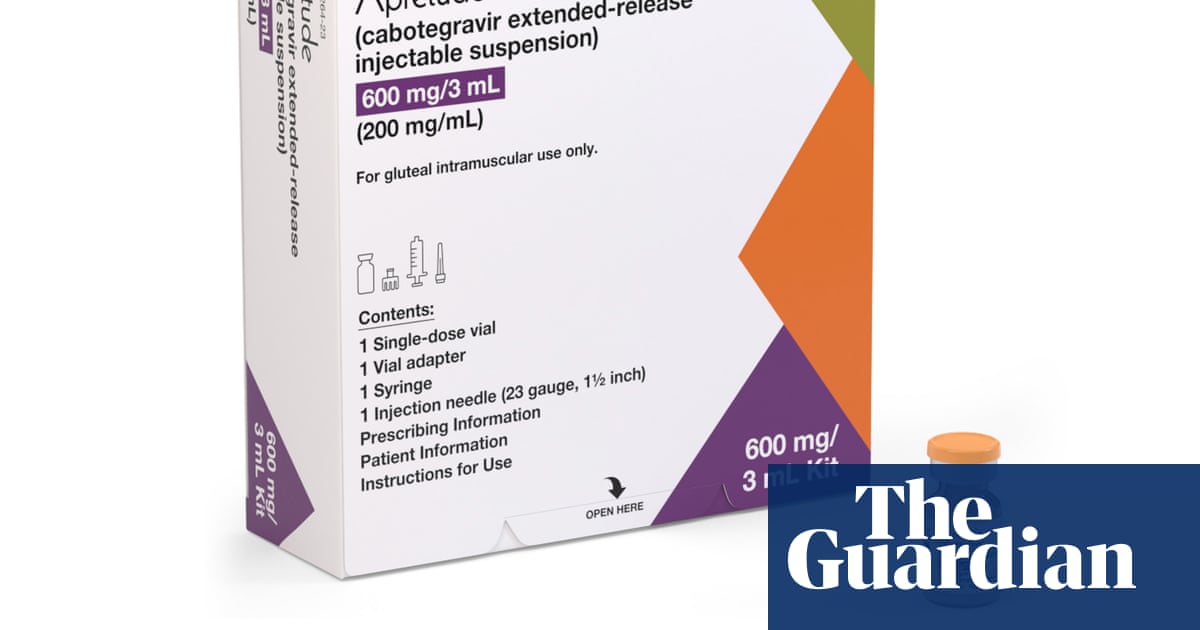
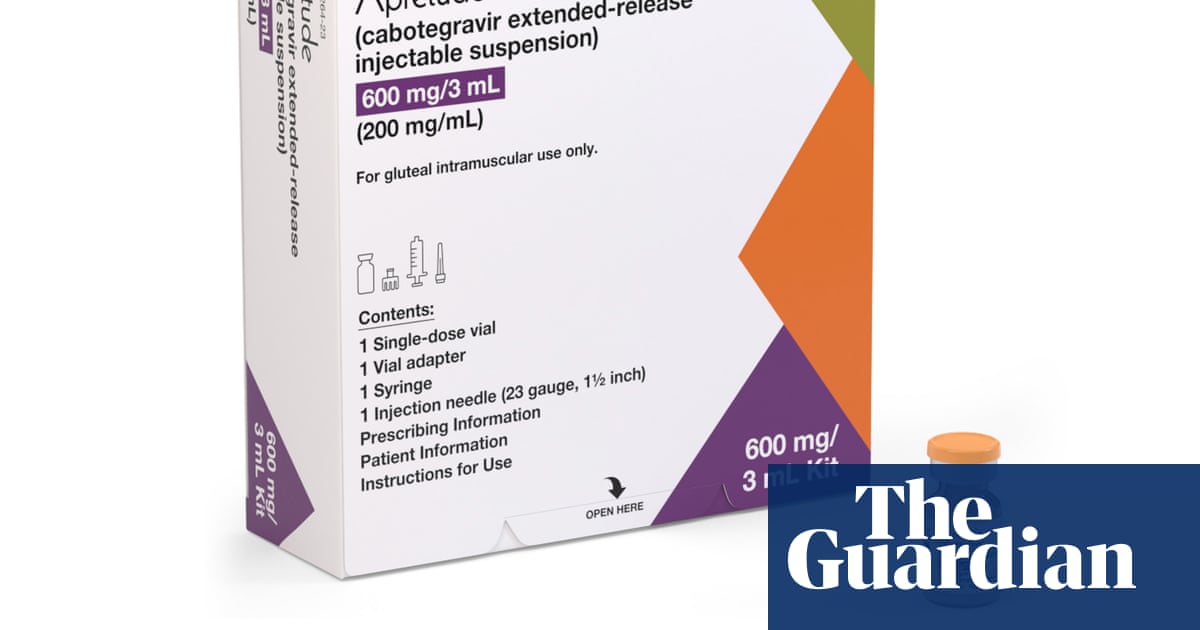
The medication, taken every eight weeks, essentially eliminates someone’s chances of contracting HIV through sex. It contains an antiretroviral drug, cabotegravir, that is released over a two-month period. The treatment is called CAB-LA (short for long-acting cabotegravir).
With more than 13% of the South African population infected with HIV, the country has the largest HIV epidemic in the world. An estimated 164,200 people in the country were infected with the virus in 2022.
The non-profit price of CAB-LA is much cheaper than in the US, where it costs about $3 700 (£2,975) for a shot, but it is still four times what South Africa’s health department pays for a daily HIV prevention pill (£2.85 for a month’s supply for each patient, according to the department).
“For CAB-LA to be cost effective to the South African government, the price would need to be within a reasonable range of oral PrEP [the daily pill], which is 129 rand [£5.68] for a two-month supply. We can’t afford to pay double or thrice the price, especially not within the context of the budget cuts our department has faced,” said the national health department’s chief director of procurement, Khadija Jamaloodien.
“What’s more”, said Jamaloodien, “is that ViiV’s non-profit price doesn’t include distribution costs, so it will be even higher than the currently quoted 540 to 570 rand per vial.”
One way of getting round CAB-LA’s high price is to allow donors such as the US government’s President’s Emergency Plan for Aids Relief (Pepfar), to pay for it. Pepfar has paid the most of any government donor for antiretroviral treatment in Africa and also funds oral PrEP in several African countries.
ViiV has already shipped Pepfar-sponsored supplies to Malawi, Zambia and Zimbabwe, which will arrive in late November, according to Mitchell Warren of the Coalition to Accelerate Access to Long-Acting PrEP. Between 2023 and 2025, Malawi is expected to receive 10,000 jabs, Zimbabwe between 10,000 and 12,000, and Zambia between 8,000 and 10,000.
Warren, and several South African HIV researchers, said Pepfar has told them that South Africa is on the list for donations in early 2024, although Pepfar has not confirmed this.
However, the health department says it is yet to decide if it will accept CAB-LA donations. Jamaloodien said the country needs to ensure that its programmes are sustainable and that relying on donations means the rollout would have to stop if the funding came to an end. In the case of HIV treatment, South Africa pays for its antiretroviral drugs itself.
“It’s certainly not something we will outright refuse, but we also need to look at sustainability,” said Jamaloodien.
In March, ViiV licensed three Indian drugmakers to produce cheaper, generic versions of CAB-LA in collaboration with the Medicines Patent Pool, a UN-backed organisation that helps poorer countries get access to medicines. One of the companies, Cipla, has a plant in Durban, where it plans to manufacture the drug.
But Cipla first needs to get the technology in place, build facilities and then run trials to prove its product works in the same way as the branded product.
Generic versions will therefore not be available until 2027 at the earliest, said Warren.
“ViiV has indicated that as volumes go up, and they get orders from large buyers like Pepfar, the Global Fund and governments like South Africa, the [non-profit] price could drop considerably,” said Warren. “We believe within the next couple of years, the branded product could cost closer to $100 or $120 for a year’s injections [as opposed to the current $175].”
But even that price would still be more than double what the daily HIV prevention pill costs the South African government, and therefore unaffordable because it won’t be cost effective, the department said.