Recent drafts of a proposed global treaty on pandemics have been widely criticized as “shameful and unjust.” When the latest round of negotiations began on March 18, it was clear that a key lesson of the COVID-19 pandemic was being ignored: that public health and the health of the economy are interdependent.
Achieving both requires rewriting the rules of how health and well-being are valued, achieved and distributed, and how economies are governed.
The success of a treaty will depend on the willingness of member states to hard-wire equity into its terms. That, in turn, will require a new economic paradigm. If the treaty is whittled down to become as inoffensive as possible, it will fail.
The World Health Organization’s Council on the Economics of Health for All, which I chaired, has already issued its recommendations for how to proceed. For starters, negotiators from all countries must remain focused on the overarching goal of preventing future health threats from becoming catastrophic. This means designing the terms of the treaty — including those related to innovation, intellectual property, public-private collaborations and funding — to be mission-oriented.
Equity must be the top priority because everyone, and every economy, ultimately suffers during a pandemic if tests, vaccines and lifesaving therapeutics are not accessible to all.
Moreover, the ways in which innovation and knowledge are governed are as critical as the innovations themselves. Governments have powerful levers for determining who benefits from innovation. They are major funders of everything from early-stage research and development to product development and manufacturing.
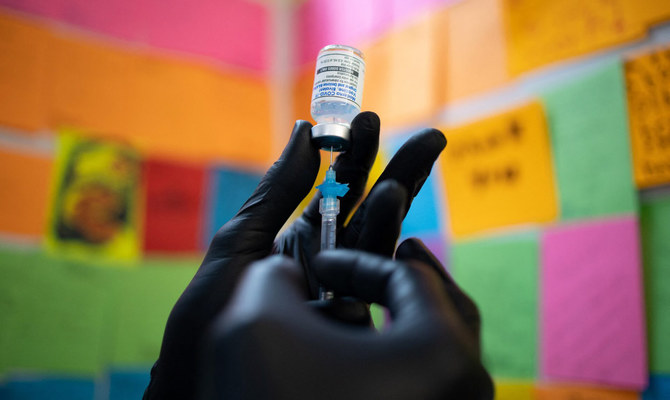
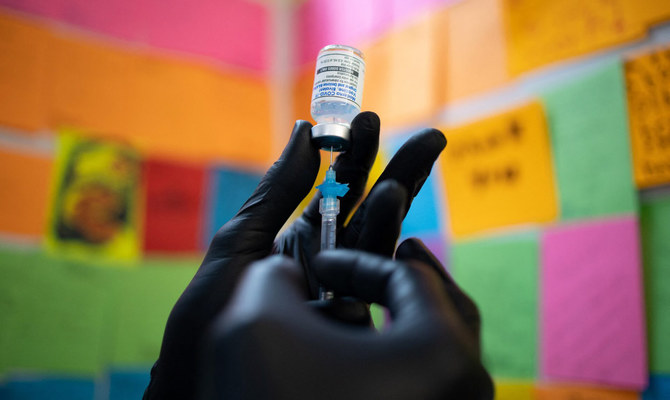
The messenger RNA COVID-19 vaccines, for example, benefited from about $31.9 billion in US public investment. Stronger conditions on private sector access to public funding would help to ensure more equitable and affordable access to the resulting products and facilitate profit-sharing and reinvestment in productive activities, such as research and development, rather than unproductive ones, such as shareholder buybacks.
The point, in each case, is to establish a more symbiotic relationship with the private sector, one based on shared goals, risks and rewards. As we saw with the repeated spread of new COVID-19 variants, a vaccine that only some can afford will not stop a pandemic. Any pandemic treaty should unapologetically commit to this shift and avoid clauses designed to serve private, rent-seeking interests.
A key part of getting public-private collaborations right is to establish an approach to knowledge governance and intellectual property rights that serves the common good, rather than protecting the profits of monopolies.
This issue has become a major flashpoint in the treaty negotiations. Lower-income countries are being asked to share pathogen data, which aids in the development of new tests, vaccines and treatments, without any guarantee they will have access to the resulting products.
To incentivize innovation and deliver broadly shared societal benefits, patents must be narrower in scope.
Mariana Mazzucato
While the current draft of the treaty alludes to the importance of intellectual property rules that do not limit affordability or access, it merely “encourages” rather than requires measures aimed at knowledge-sharing and limiting royalties. Even weak language that asks governments to “consider supporting” patent waivers has become a sticking point.
This suggests that a misplaced drive to preserve current intellectual property rules is complicating the negotiations. To incentivize innovation and deliver broadly shared societal benefits, patents must be narrower in scope; they must encourage productive follow-on innovation and collective intelligence; and they must be accompanied by commitments to transfer the knowledge and technology required for production.
Another obstacle to the success of the pandemic treaty is the fact that it currently seems to be delinked from clear funding commitments. The International Monetary Fund estimates that the global economy suffered losses of at least $13.8 trillion when COVID-19 lockdowns and supply-chain disruptions tipped the world into recession. Governments then spent trillions more responding to the crisis.
It should be obvious that scaling up investments in prevention is preferable, in terms of health, prosperity and justice, to incurring the costs arising from a crisis that has already spun out of control. As the WHO council pointed out: “It is more cost effective to prevent than to cure.”
The quality of financing is as important as its quantity. Lower-income countries need long-term financing for critical investments in health. The treaty’s nod to the importance of debt relief in helping to free up fiscal capacity for pandemic prevention, preparedness and response is welcome but the language is worryingly noncommittal.
Financing for health must be understood as a long-term investment, rather than as a cost that can be reduced to serve short-sighted budget targets. It is also a responsibility that transcends national borders.
Lastly, since the scope of the pandemic treaty cuts across government ministries and sectors, the issue of health should not be left solely to health ministries. Health is massively affected by economic policy choices, such as those related to intellectual property rights, and decisions made across government affect the social, environmental and economic determinants of health.
Governments, across all ministries, can and should redesign how innovation is governed, how the public and private sectors relate to one another and how finance is structured to shape markets in the interests of human and planetary health. Failure to prioritize “health for all” will have far-reaching ramifications for the resilience and stability of economies worldwide.
As member states cavil over clauses, removing references to health as a human right and watering down intellectual property restrictions, financial commitments and monitoring provisions, there should be no ambiguity about the choice they face.
Centering the treaty on the goal of preventing or minimizing pandemics would compel policymakers to see this clearly and to abandon the myopic assumptions that have limited international and public-private collaborations.
As member states prepare for the World Health Assembly in May, this imperative should be front of mind.
• Mariana Mazzucato, founding director of the UCL Institute for Innovation and Public Purpose, is chair of the World Health Organization’s Council on the Economics of Health for All.
©Project Syndicate