It is 11 days since I gave birth to my first baby. My breast milk still hasn’t “come in” properly and no one can tell me why. Midwives come and go, looking at me sympathetically and telling me to feed on demand, pump whenever I can and top up with formula milk. Still, I have no idea how I am going to exclusively breastfeed my child, which is what all the advice recommends.
Sleepless, anxious and desperate, I do what many others with the privilege of disposable income do in this situation and pay for a private consultant. I find a local International Board certified lactation consultant (IBCLC) online and we meet. She diagnoses my son with tongue-tie, which she treats by snipping the skin connecting his tongue to the bottom of his mouth. She also suggests that I start taking a drug I have never heard of, domperidone, to help me produce more milk.
The drug is usually prescribed as an anti-sickness drug, but is used off-label – particularly in Canada and the US, but also increasingly in the UK – to induce or increase lactation, she explains. It is quite common and safe to use, she says, but GPs are hesitant to prescribe it for this purpose because the UK’s healthcare system is “behind” when it comes to breastfeeding. She took it herself, to breastfeed her twins, and is confident that a letter from her will convince my GP that I need it.
She is right; my GP prescribes it without any consultation and I take the first pill as soon as I get my hands on it. The prescription is 10mg, three times a day for seven days, which is the NHS’s maximum recommended dose for nausea. I feel fortunate. Everything is going to be OK.
But it isn’t. I make barely any more milk and pay for yet more expensive specialists to tell me that the latch is “good”, but they cannot explain why my son is still not getting enough. People comment on how “skinny” he looks. After he drops two weight centiles, a health visitor tells me he is in danger of “falling off the charts”. I am getting more anxious by the day.
Around this time, my husband and my best friend – who is a therapist – express concern about my declining mental health. I have a history of obsessive compulsive disorder and anxiety, so their apprehension is well placed. They gently propose adding more formula into my son’s diet. But these discussions call for a level of rationality I cannot provide.
Instead, I ask my GP for breastfeeding-safe antidepressants, which seems like the quickest fix until I have time to make long-term changes that might improve my mood. After all, what does it matter how I am doing? What is my role as a mother if not to sacrifice my needs for my child? The tablets are dispensed after a short telephone appointment.
The World Health Organization recommends that babies are breastfed exclusively from “within the first hour of birth” until six months. After this, it advises feeding from the breast alongside the introduction of solid foods “for up to two years and beyond”. These recommendations are echoed by the NHS.
Still, according to Unicef, the UK has one of the lowest breastfeeding rates in the world. The reasons for this are myriad, but a decline in support for new mothers is a big factor. “For some women, breastfeeding may be more difficult,” says Birte Harlev-Lam, a midwife and executive director at the Royal College of Midwives. “Trying to sustain it without the right support can be detrimental to a woman’s mental health.” In 2015, research from the University of Seville, using data from women in Britain, found that those with the highest risk of developing postnatal depression were women who had planned to breastfeed and had been unable to do so.
My original lactation consultant said she had taken 120mg of domperidone a day – four times my dose – to breastfeed her twins, so I look into other ways of getting hold of the drug. I order it via online pharmacies, which dispense it for my fake “travel sickness” at 30mg a day for up to seven days (although the online pharmacies give me 10 days’ worth). I need more, so I order it in the name of pretty much everyone I am close to and build up a stash. I increase my dose to 60mg a day and then 90mg a day, based on the protocol published by the International Breastfeeding Centre in Canada.
Unsupervised self-medicating is not something I have done before – but I am not alone in being led to it by a desire to breastfeed. Maria, from North Yorkshire, says she was advised by an IBCLC to access the drug via a Facebook breastfeeding support group, which illegally imports and sells domperidone from foreign pharmacies. “The pressure to feed my child set off a spiral of events,” she says. “I wish I knew then that it wasn’t worth it.”
Elyse, an NHS worker in Sussex, says she bought domperidone illegally and took 120mg a day. She says that she would “never in a million years” have bought a drug online off-label before she struggled with breastfeeding. “We are so desperate to do the best for our babies that we will just do anything,” she says.
My milk supply does increase, but I soon run out of pills again. Another IBCLC points me in the direction of a private doctor in London who is willing to prescribe the drug off-label. After a £170 phone consultation, I get a prescription for thousands of pills (for £67). The only side-effects mentioned relate to my heart, so I have a private ECG to check it (another £50). Under the supervision of the private doctor, my dose is increased to 120mg a day and then to 160mg a day over the course of a few weeks.
But my mental state is getting worse – and so is breastfeeding. Although I have spent a large chunk of my savings – and poured hundreds of hours into pumping, feeding and desperately searching for solutions online – my son, at 10 weeks old, refuses to breastfeed. My domperidone dose is more than five times what the NHS recommends. I am producing slightly more milk, but it is not consistent. I battle on for two more painful weeks before I admit to myself that I have failed.
I email the private doctor to let them know that I will be stopping the domperidone. The doctor responds to say they are sorry it didn’t work out. The email contains no advice about coming off the drug, so I simply stop taking it the next day.
About five days later, my emotional state worsens. I cry for hours at a time and I have panic attacks. I become convinced that I am not fit to take care of my son and that I will cause him harm. I call his dad and beg him to come home. I call 999, too, but hang up before I get through. I am too scared to admit to a stranger that I might be losing touch with reality. I am terrified that any professional I tell might take him away from me.
At this point, I am not sure if I have developed postnatal depression in the fourth trimester – which is common, especially for those with previous mental health problems – but I am certain that coming off the domperidone has exacerbated my low mood and anxiety. I write to the private doctor and ask if what I am feeling could be a side-effect of stopping the drug.
They ring me soon after and worriedly explain that domperidone, especially at such a high dose, is not something you can just stop taking; you need to taper off it slowly. Withdrawal can cause anxiety and depression. For a small number of people, so can taking the drug in the first place.
This is the first I have heard about mental health side-effects. The private doctor apologises for not warning me. They tell me to go back on a dose of 120mg a day and wean off one pill a week until I am down to zero.
This sounds simple enough. But what follows is the darkest period of my life. I contemplate suicide – something I have never considered before. I am referred to a psychiatrist with my local perinatal mental health service to support me in crisis and assist me in the tapering-off process. In all her many years in this job, she says, she has never come across anyone taking domperidone at my dosage. She consults an NHS pharmacologist who says the same.
As a result, she can guide me, but she won’t be able to advise me on how each step will affect me psychologically. I am unable to see a way out and none of the professionals I am in contact with can say with confidence when I will find one. My antidepressant prescription is increased, then again – seven times.
According to Prof Parastou Donyai, the Royal Pharmaceutical Society’s chief scientist, domperidone works by blocking dopamine receptors, which has been found “to increase the release of prolactin [the milk-making hormone] in the body, leading to increased milk production”. Because of this, Donyai explains, the drug is sometimes prescribed to breastfeeding mothers who are experiencing difficulties with milk supply. However, she is quick to caution that, in the UK, domperidone is licensed only for use in the treatment of nausea and vomiting, information that is consistent with the NHS website, where no mental health side-effects are noted.
Dr Mark Horowitz, a clinical research fellow in psychiatry at North East London NHS foundation trust, specialises in coming off psychiatric drugs. Over the years, he says, he has been contacted by several women who have been prescribed domperidone to aid lactation and have later had trouble coming off it. “In the literature on domperidone, there are cases that include people becoming agitated, anxious, hallucinating, being depressed and becoming suicidal,” he says.
They are women like Gemma, from Hertfordshire, who not only reported similar side-effects to me, but had also seen the same private doctor and was taking 90mg a day. While trying to come off the drug, she says, she experienced anxiety, depression and “raging insomnia” for months. She describes it as “a truly awful experience” that resulted in her being unable to look after her son on her own for two weeks.
According to Prof Kamila Hawthorne, the chair of the Royal College of GPs, “most GPs would not prescribe it for breastfeeding”. If they did, “they would need to explain [to the patient] that the medication was not licensed for this purpose and clearly explain these side-effects to their patient, so that she can give informed consent if she wants to go ahead”.
My private doctor declined to comment for this article. The International Board of Lactation Consultant Examiners also declined to comment, but referred to a document on its website in which it confirmed that IBCLCs are not medical practitioners, but have a duty to “act with reasonable diligence by making necessary referrals to other health care providers and community support resources when necessary”.
While the International Breastfeeding Centre does provide information about tapering off domperidone, health bodies in Canada have raised concerns about the drug. In April, the College of Physicians and Surgeons of Ontario upheld a complaint by a woman who had severe psychological withdrawal effects after being prescribed it by a doctor.
Despite my experience, I have spoken to dozens of women who have described domperidone as a “wonder drug” that has enabled them to breastfeed their babies with minimal side-effects. Most of those were prescribed it by their GP or a consultant in a neonatal intensive care unit. Only about half of them have said they were warned about its potential side-effects and the need to taper off the drug slowly.
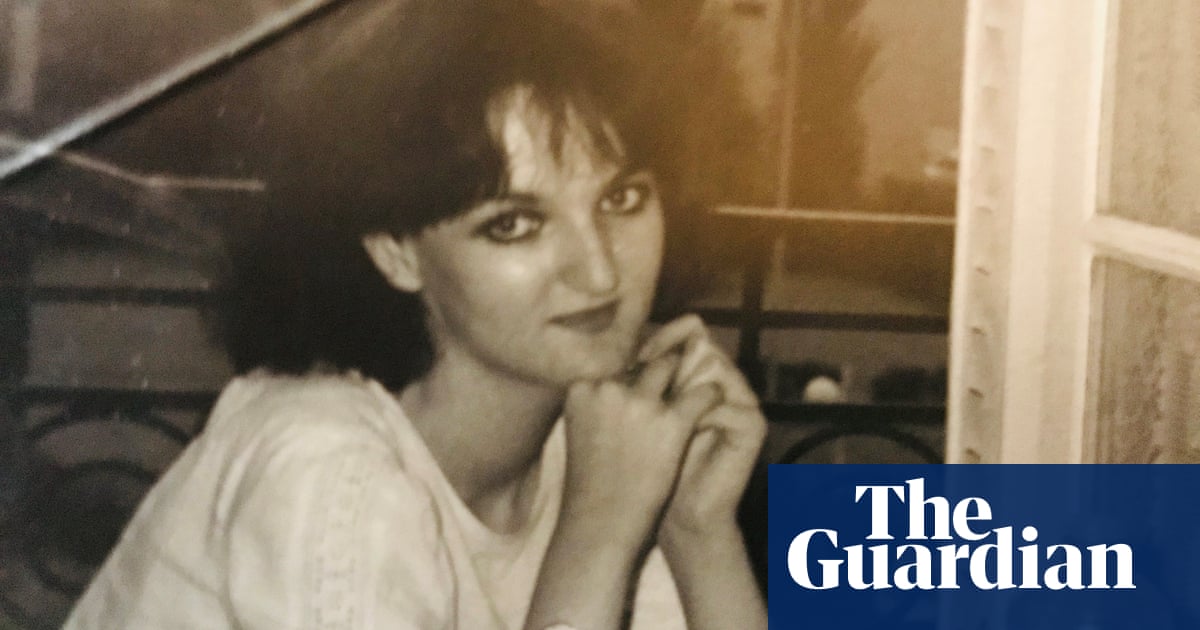
I finally stopped taking domperidone just before my son’s first birthday. The night before, I cried for hours. There have been many joyful moments, but, looking at the hundreds of photos of us together in that first year, I can see the pain beneath my smile.
I am pregnant again. This time, I will establish boundaries about how I approach breastfeeding and when I will give up if it isn’t working. It has taken a lot of hard work to get here, but I am confident that, whichever way I end up feeding my next baby, we will both be OK.
Some names have been changed
In the UK and Ireland, Samaritans can be contacted on freephone 116 123, or email jo@samaritans.org or jo@samaritans.ie. In the US, you can call or text the National Suicide Prevention Lifeline on 988, chat on 988lifeline.org or text HOME to 741741 to connect with a crisis counselor. In Australia, the crisis support service Lifeline is 13 11 14. Other international helplines can be found at befrienders.org
Do you have an opinion on the issues raised in this article? If you would like to submit a response of up to 300 words by email to be considered for publication in our letters section, please click here