Genetically modified bacteria could be used to treat intractable lung infections, according to research aiming to combat the threat of antibiotic resistance.
The research, in mice, showed that a re-engineered bacteria could be used to target drug-resistant infections and make them susceptible to antibiotics that would otherwise be ineffective.
Dr Maria Lluch, of the International University of Catalonia and senior author, described the treatment as a “battering ram that lays siege to antibiotic-resistant bacteria”.
“The treatment punches holes in their cell walls, providing crucial entry points for antibiotics to invade and clear infections at their source,” said Lluch. “We believe this is a promising new strategy to address the leading cause of mortality in hospitals.”
The bacteria-based treatment doubled mouse survival rate compared with not using any treatment, according to the research carried out at the Centre for Genomic Regulation in Barcelona. Administering a single, high dose of the treatment showed no signs of toxicity in the lungs. Once the treatment had finished its course, the immune system cleared the modified bacteria in a period of four days.
Antimicrobial resistant infections pose a growing threat, directly accounting for at least 1.27 million deaths each year, according to figures released this month, meaning there is an urgent need for alternative treatments. The latest work follows a clinical breakthrough last year in the use of modified viruses, known as phages, to attack bacterial infections.
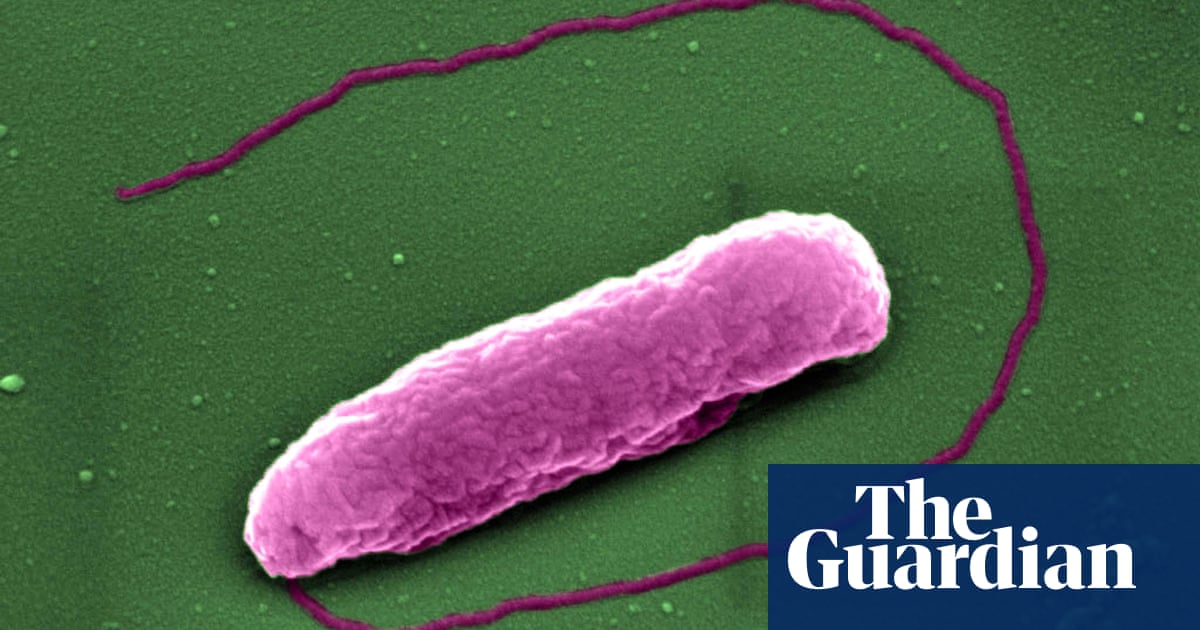
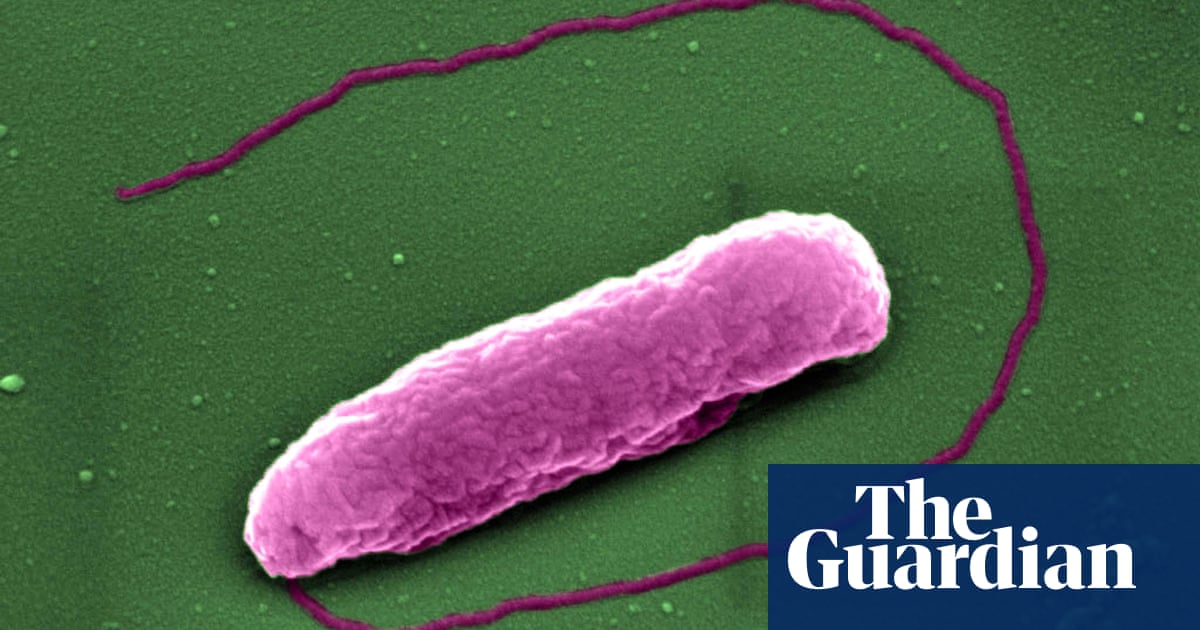
The latest treatment was designed to target Pseudomonas aeruginosa, which can lead to intractable infections because the bacteria form biofilms. These can attach themselves to surfaces in the body, forming impenetrable structures that escape the reach of antibiotics. Biofilms can also grow on the surface of endotracheal tubes used by critically ill patients who require mechanical ventilators to breathe.
This causes ventilator-associated pneumonia (VAP), a condition that affects up to one in four patients who require intubation and about half those intubated due to severe Covid-19. VAP kills up to one in eight patients.
The study, published in the journal Nature Biotechnology, used a genetically engineered version of Mycoplasma pneumoniae, removing its ability to cause disease (mild respiratory illness) and repurposing it to produce toxins designed to kill or inhibit the growth of Pseudomonas aeruginosa. The team plan to carry out further research before moving on to clinical trials. In future, they envision the treatment being administered using a nebuliser, allowing the patient to inhale the bacteria in a mist.